The fountain of youth isn’t hidden in some exotic location or expensive serum—it’s in how you manage your daily stress.
While we’ve long known that stress affects our mood and energy, cutting-edge science reveals something far more profound: chronic stress literally ages us at the cellular level, stealing years from our lives and vitality from our years.
So here are a few questions to ask yourself:
- How often do you feel stressed?
- How do you cope with stress?
- And most importantly, what can you do to manage your stress levels and slow down the aging process?
Stress is an inevitable part of life. We all experience it in various forms and at different intensities. It could be pressure from work, financial worries, family conflicts, or even just day-to-day tasks piling up.
But did you know that chronic stress can have a significant impact on our physical health as well? And did you know it could be altering your very DNA?
Telomeres & Time: The Cellular Science Behind Stress and Aging
Inside every cell of your body, protective caps called telomeres sit at the ends of your chromosomes like plastic tips on shoelaces, preventing your DNA from unraveling.
Each time a cell divides, these telomeres get slightly shorter. When they become too short, cells can no longer divide properly and either die or become dysfunctional – a process directly linked to aging and disease.
Dr. Elizabeth Blackburn’s Nobel Prize-winning research revolutionized our understanding of cellular aging by discovering telomerase, the enzyme that maintains and repairs telomeres.
Her groundbreaking work revealed that telomere length isn’t just a passive marker of aging but an active player in determining how quickly we age and how susceptible we become to age-related diseases. This discovery transforms aging from an inevitable decline into a process we can influence through lifestyle choices, particularly stress management.
How Stress Hijacks Your Cellular Clock
Chronic stress acts like a cellular accelerant, dramatically speeding up telomere shortening.
Research shows that people experiencing high levels of chronic stress can have telomeres equivalent to someone a decade older.
This isn’t just correlation – studies demonstrate that stress hormones directly damage telomeres and suppress telomerase activity, creating a double assault on cellular longevity.
The implications are staggering. Shortened telomeres correlate with increased risk of heart disease, cancer, diabetes, and premature death.
One study found that women caring for chronically ill children – a situation of intense, prolonged stress – showed telomere shortening equivalent to 10 years of additional aging compared to low-stress controls.
This cellular damage translates directly into real-world health outcomes, with shortened telomeres predicting mortality risk more accurately than chronological age alone. That’s a testament to the power and importance of managing stress levels in our daily lives.
The Cascade Effect
Telomere damage doesn’t occur in isolation.
As telomeres shorten, cells enter a state called senescence – they stop dividing but don’t die, instead secreting inflammatory compounds that damage surrounding healthy cells.
This creates a cascade of cellular dysfunction that accelerates tissue aging throughout the body. Organs function less efficiently, skin loses elasticity, immune response weakens, and disease risk skyrockets.
Knowing this mechanism highlights why a mental health platform focused on stress reduction isn’t just about feeling better emotionally – it’s about protecting the very building blocks of life.
Every stressful day without adequate recovery literally ages us at the molecular level, making stress management not a luxury but a biological necessity.
Cortisol Overload: When Your Stress Hormones Turn Against You
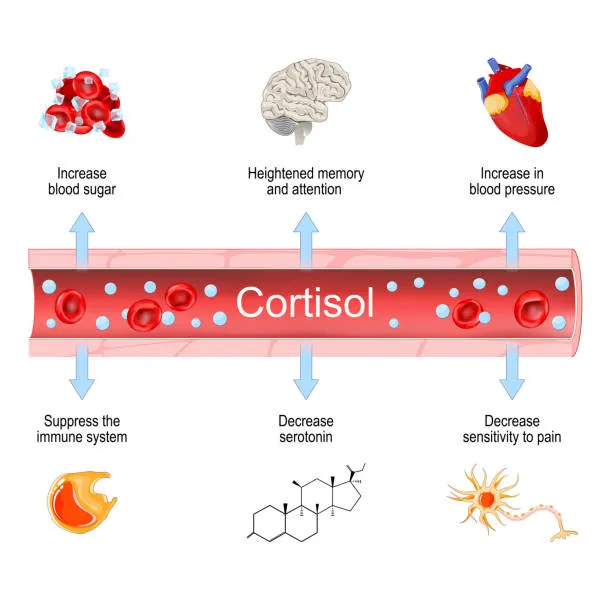
Cortisol, often called the stress hormone, plays a pretty important role in helping us respond to immediate threats.
It’s like a spark to fuel – it mobilizes energy, sharpens focus, and temporarily suppresses non-essential functions like digestion and reproduction.
This system works brilliantly for short-term challenges. But when stress becomes chronic, cortisol levels remain elevated far beyond their intended duration, transforming from protector to destroyer.
Prolonged cortisol elevation triggers widespread biological disruption. It promotes visceral fat accumulation, particularly around the midsection, creating the dangerous “apple shape” body type associated with metabolic syndrome.
This isn’t just an aesthetic concern – belly fat acts as an endocrine organ, producing inflammatory compounds that further accelerate aging.
Cortisol also breaks down muscle tissue for energy, leading to sarcopenia (age-related muscle loss) that typically doesn’t begin until much later in life.
The Inflammatory Cascade
Chronic cortisol exposure creates a pro-inflammatory state throughout the body.
Inflammation, while essential for healing acute injuries, becomes destructive when chronic. This persistent inflammation damages blood vessels, accelerating atherosclerosis and increasing heart disease risk.
It disrupts insulin signaling, promoting diabetes. It even crosses the blood-brain barrier, contributing to neuroinflammation linked to depression, anxiety, and cognitive decline.
The immune system suffers particularly under chronic cortisol exposure. While acute stress temporarily boosts immune function, chronic stress suppresses it, leaving us vulnerable to infections, slow wound healing, and even reduced vaccine effectiveness.
This immunosuppression also impairs the body’s ability to identify and destroy abnormal cells, potentially increasing cancer risk. A personal growth platform that teaches stress management techniques becomes a tool for immune system preservation.
Hormonal Chaos
Cortisol doesn’t act alone. It disrupts the entire endocrine system.
Chronic elevation interferes with thyroid hormones, slowing metabolism and promoting weight gain. It suppresses growth hormone and testosterone, accelerating muscle loss and reducing bone density. In women, it disrupts estrogen and progesterone balance, affecting everything from menstrual cycles to mood stability.
This hormonal disruption creates a vicious cycle.
Poor sleep quality from cortisol elevation leads to increased hunger hormones, driving overeating and further metabolic dysfunction.
Reduced sex hormones affect mood and motivation, making it harder to engage in stress-reducing activities like exercise or social connection.
Breaking this cycle requires comprehensive approaches that address both stress and its downstream hormonal effects.
Your Brain on Stress: Cognitive Decline and Emotional Burnout
The Shrinking Hippocampus
The hippocampus, your brain’s memory center, is particularly vulnerable to chronic stress.
Studies using brain imaging show that people with chronic stress have measurably smaller hippocampi, with volume reductions of up to 14% in severe cases.
This isn’t just correlation. Animal studies confirm that stress hormones directly kill hippocampal neurons and suppress the growth of new ones.
This hippocampal atrophy manifests as memory problems that go beyond normal forgetfulness.
People experience difficulty forming new memories, struggle with spatial navigation, and lose the ability to distinguish between similar experiences – a phenomenon called pattern separation that’s crucial for accurate memory formation.
These changes mirror those seen in early Alzheimer’s disease, and indeed, chronic stress is now recognized as a significant risk factor for dementia.
The Overactive Amygdala
While the hippocampus shrinks, the amygdala (your brain’s fear center) becomes hyperactive under chronic stress.
This creates a brain primed for threat detection, seeing danger where none exists. The overactive amygdala hijacks rational thinking, making it difficult to assess situations objectively or regulate emotional responses appropriately.
This amygdala overdrive goes beyond just affecting mood. It can fundamentally alter how we process information and make decisions.
Studies show that chronic stress shifts decision-making from the thoughtful prefrontal cortex to the reactive amygdala, leading to impulsive choices and poor judgment.
This explains why stressed individuals often make decisions that perpetuate their stress, creating self-reinforcing cycles of poor choices and negative outcomes.
Mental health education that explains these mechanisms helps people understand their stress responses aren’t character flaws but biological reactions that can be modified.
Accelerated Brain Aging
The combination of hippocampal atrophy, amygdala hyperactivity, and chronic inflammation creates a perfect storm for accelerated brain aging.
People in their 30s and 40s with chronic stress show cognitive decline patterns typically seen in much older adults.
Processing speed slows, executive function deteriorates, and mental flexibility decreases. These are all hallmarks of an aging brain appearing decades early.
Neuroimaging studies reveal that chronic stress accelerates brain age by an average of four years, with some individuals showing brain ages ten years older than their chronological age.
This premature brain aging is associated with increased risk of neurodegenerative diseases, stroke, and mental health disorders.
A healthy lifestyle community that prioritizes stress reduction becomes essential for preserving cognitive function across the lifespan.
Reversing the Clock: How Nervous System Regulation Slows Aging
The most exciting discovery in stress and aging research is that damage isn’t permanent.
Studies show that stress-reduction interventions can actually lengthen telomeres and reverse some cellular aging markers.
Dr. Blackburn’s research found that people who practiced meditation for just 12 minutes daily showed increased telomerase activity within weeks, with some participants showing telomere lengthening after several months of practice.
Exercise emerges as particularly powerful for cellular renewal. Moderate aerobic exercise increases telomerase activity by up to 200%, while also promoting the production of brain-derived neurotrophic factor (BDNF), often called “Miracle-Gro for the brain.”
This combination protects existing neurons while promoting the growth of new ones, particularly in the stressed hippocampus. Even walking for 30 minutes daily can measurably slow cellular aging within months.
Daily Rituals for Nervous System Healing
Creating a daily practice for nervous system regulation doesn’t require hours of meditation or expensive interventions.
Simple slowing movements and breathwork techniques like box breathing (4-4-4-4 count breathing pattern) activate the parasympathetic nervous system within minutes, countering stress-induced sympathetic overdrive.
Progressive muscle relaxation before bed improves sleep quality while reducing nighttime cortisol levels.
Social emotional learning plays a crucial role in stress resilience. Learning to identify and label emotions reduces amygdala reactivity, while developing emotional regulation skills prevents stress spirals.
These skills, once thought to be fixed in childhood, show remarkable plasticity even in adults. Regular practice of emotional awareness and regulation can rewire stress response patterns within weeks.
The Power of Connection
Social connection emerges as one of the most powerful anti-aging interventions available.
Studies show that strong social bonds can add seven years to life expectancy – more than quitting smoking. Social support buffers stress hormones, with research showing that simply holding a loved one’s hand reduces cortisol response to stressors by up to 50%.
Building and maintaining social connections requires intentionality in our increasingly isolated world. Joining groups aligned with personal interests, volunteering for causes that matter, or participating in community activities creates natural opportunities for connection.
A platform for social impact that combines stress reduction with community engagement addresses both individual and collective well-being, creating positive feedback loops where helping others reduces personal stress while building social bonds.
Sleep: The Ultimate Recovery Tool
Quality sleep represents the body’s primary recovery period from daily stress. During deep sleep, the brain’s glymphatic system removes metabolic waste, including proteins associated with Alzheimer’s disease.
Growth hormone peaks during sleep, repairing tissues damaged by daytime cortisol. The brain consolidates memories and processes emotions, preventing the accumulation of psychological stress.
Yet chronic stress severely disrupts sleep architecture, creating another vicious cycle. Breaking this cycle requires sleep hygiene practices: consistent sleep schedules, cool dark rooms, and avoiding screens before bed.
Cognitive behavioral therapy for insomnia (CBT-I) shows remarkable effectiveness, with improvements in sleep quality translating directly to reduced inflammatory markers and improved telomerase activity.
It’s Time to Start Seeing Stress Resilience as Life Extension
The science is clear: chronic stress ages us rapidly at every level, from our DNA to our organs to our brains.
But equally clear is our remarkable capacity for renewal.
Unlike chronological aging, stress-induced aging is largely reversible through accessible interventions that anyone can implement.
The key lies not in eliminating stress – an impossible goal in modern life – but in building resilience and recovery capacity.
This means developing a toolkit of stress-management techniques, creating supportive social networks, and prioritizing recovery activities like sleep and exercise.
It means understanding that time spent on stress reduction isn’t selfish but essential for longevity and quality of life.
Ready to slow down your biological clock? Join AlignUs to access evidence-based tools, a supportive community, and expert guidance for managing stress and optimizing longevity.
Together, we can reverse the effects of aging and live our healthiest, happiest lives.